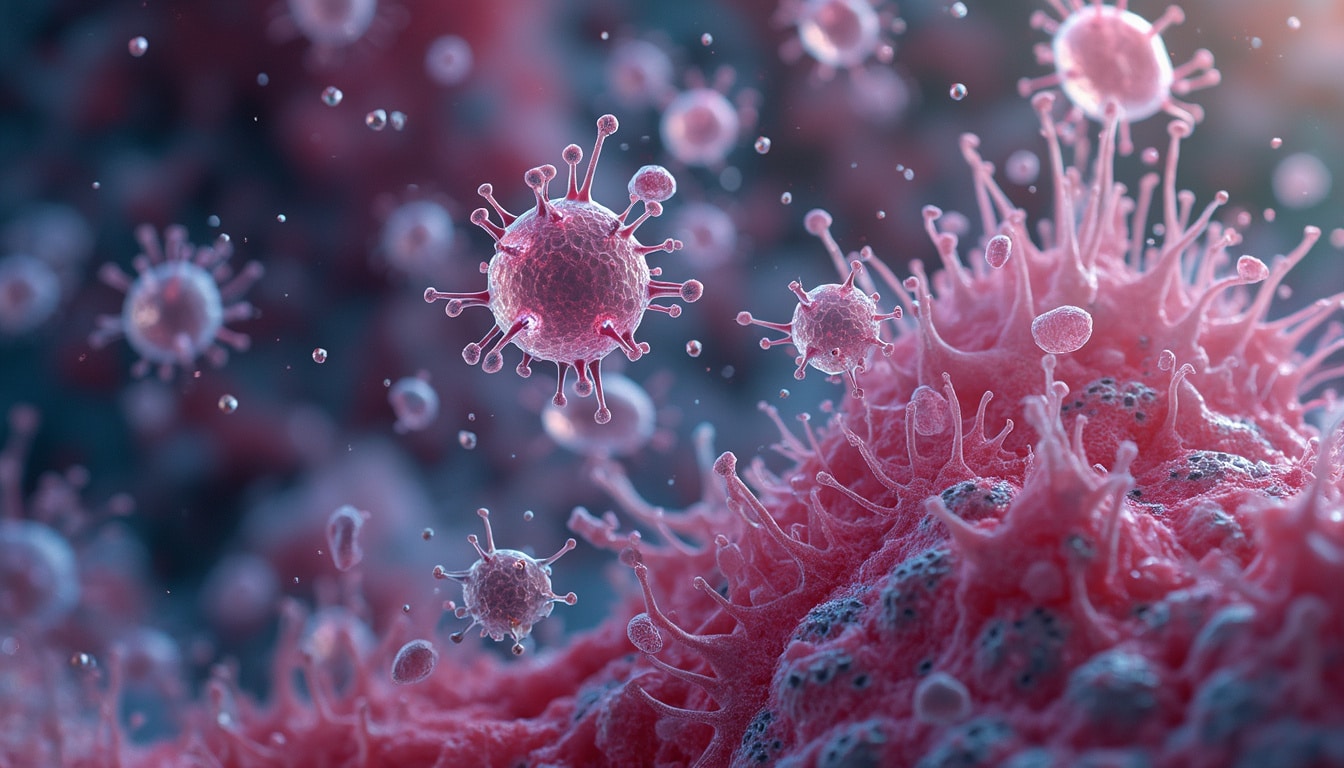
Benign prostate hyperplasia (BPH), a frequent age-related condition in men, involves the enlargement of the prostate gland over time. Its precise causes remain elusive, particularly how age-associated changes in immune cells contribute to its development. Recent studies highlight a specific population of CD8+ T cells, marked by high Granzyme K and low Granzyme B expression, which infiltrate aging prostates. This subpopulation’s presence correlates with worsening symptoms, possibly signaling a connection to immune aging. Furthermore, the encouragement of senescent behavior by these T cells may link prior infections and inflammation of the prostate to increased risks, hinting at complex interactions between the immune system and prostate health as men age.

Table of Contents
Togglea novel t-cell population associated with aging
As men age, the intricacies of their cellular biology become ever more pronounced. Benign prostatic hyperplasia (BPH), a prevalent non-cancerous enlargement of the prostate, becomes a growing concern. It is often tied to age-related cellular developments. Recent research highlights an intriguing link between BPH and a specific subset of T cells, which tends to evolve with age. This discovery … provides insight into the underlying mechanisms lingering in the body as time passes, revealing a more complex interplay between immune function and age.
The presence of these specialized CD8+ T cells is characterized by unique gene expressions—namely, elevated Granzyme K and reduced Granzyme B levels. As they infiltrate into the aged prostate, they seem to embody a hallmark of immune aging. Their accumulation might not only align with the development of BPH but may also trigger symptomatic expressions that disrupt daily life. The narrative unfolds as scientists aim to map and understand these pathways deeply to anticipate and control the swelling of the prostate.
immune aging and the rise of prostatitis
Notably, prior infections and prolonged states of inflammation—collectively termed as prostatitis—heighten the risk of developing BPH in later years. The aging immune landscape, with its inflammatory overtones, can provoke and exacerbate prostate conditions. Such dynamics primarily involve the interplay between senescent cells and inflammatory cytokines that may perpetuate harmful prostatic changes. The interaction between these cells and sentient immune responses remains under the microscope as researchers explore interventions.
therapeutic insights into bph and immune modulation
Ongoing studies suggest promising lines of inquiry by targeting the unique immune paradigms observed in BPH patients. By modulating senescence-associated secretory phenotypes, the potential for alleviating BPH symptoms could rise, paving the path towards innovative therapeutic solutions. Single-cell RNA sequencing has uncovered an accruement of pertinent data, enabling more nuanced tracking of cellular changes and providing a scaffold for potential clinical interventions. These insights elicit a hopeful outlook on managing BPH by strategically manipulating immune components.