The silent yet tumultuous journey of atherosclerosis takes a sharp turn when entangled with Type 2 diabetes. Though our arteries silently weave a tapestry of fatty plaques, the introduction of diabetes adds a dangerous twist to the narrative. The lurking presence of lipid-laden plaques, portrayed as ticking time bombs, adopt a more deceitful character in the shadows of diabetes. By intricately altering the delicate balance and potency of these arterial impostors, Type 2 diabetes reshapes them into more perilous formations, amplifying the threat of heart attacks and strokes. This interplay, driven by intricate metabolic conversations, underscores a dire need to unravel the mysteries of how high blood sugar steers these arterial saboteurs towards chaos.
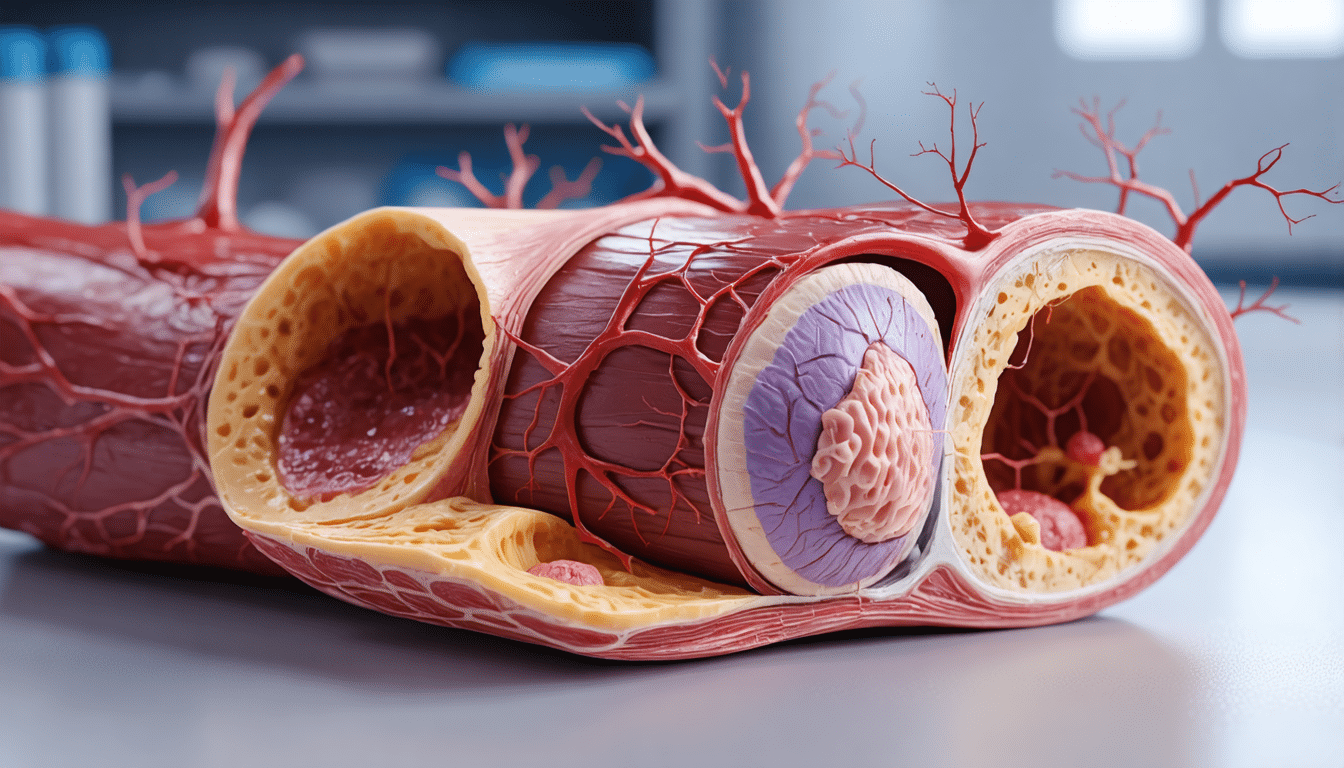
Atherosclerosis is characterized by the buildup of fatty plaques in the walls of blood vessels, which can obstruct blood flow. The stability of these plaques plays a crucial role in their potential danger. Plaques rich in lipids are more prone to rupture, potentially causing a heart attack or stroke. In contrast, plaques with fibrotic or calcified structures are considered less risky. Recent research highlights that metabolic diseases, such as Type 2 Diabetes, worsen cardiovascular disease by affecting the stability of these plaques.
Studies reveal that individuals with Type 2 Diabetes have plaques with lower levels of collagen, potentially leading to increased instability. The presence of transforming growth factor-ß is notably lower in diabetes patients, correlating with cardiovascular events. This growth factor, primarily sourced from vascular smooth muscle cells, supports collagen formation and cell differentiation and is influenced by hyperglycemia. Understanding the role of transforming growth factor-ß2 in fibrous repair offers promising avenues for therapeutic strategies.
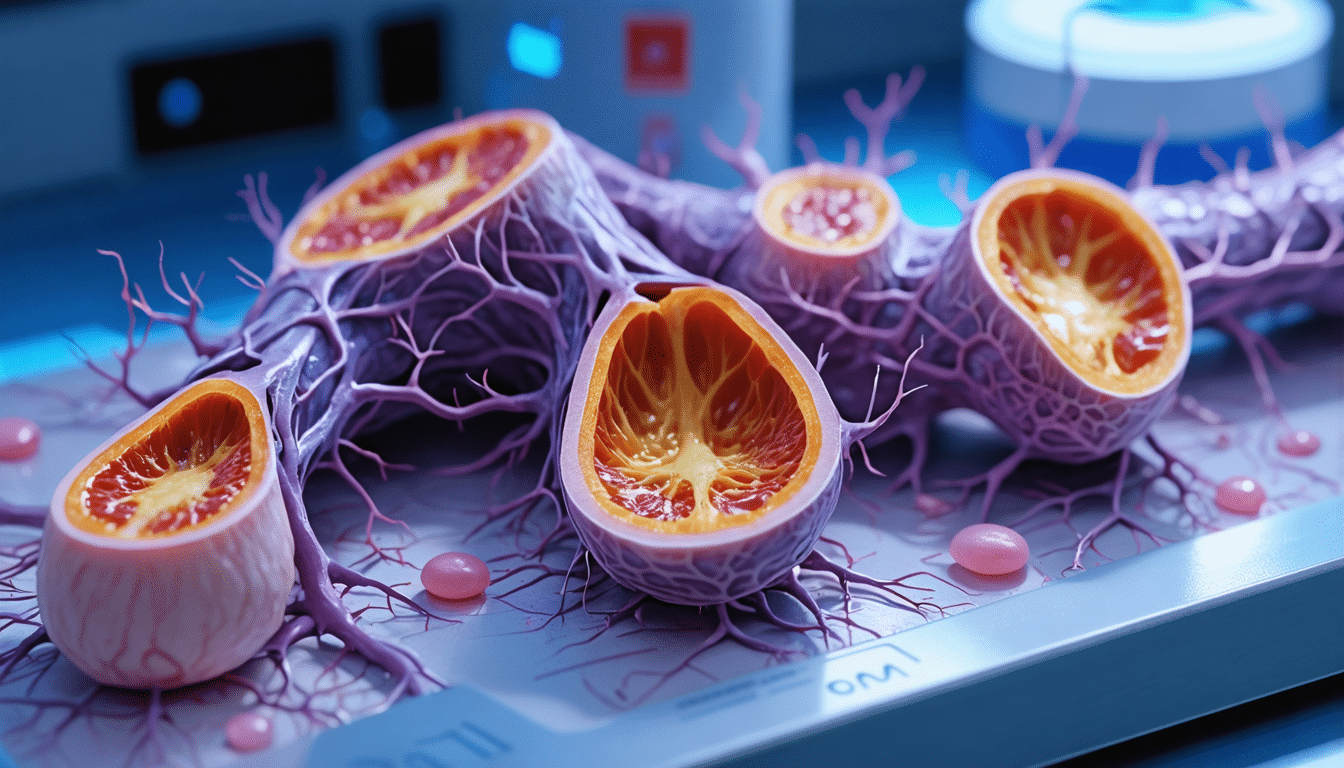
Table of Contents
Toggletype 2 diabetes and atherosclerosis interplay
Atherosclerosis, a stealthy threat within our blood vessels, often evolves insidiously as fatty plaques settle along the arterial walls. In the presence of type 2 diabetes, the scenario complicates further. The nature and stability of these plaques undergo transformative changes, paving pathways often laden with peril. This disease doesn’t only inflame arteries; it tempers the core stability of the plaque itself, revealing a hidden menace where seemingly benign cholesterol deposits evolve into ticking time bombs. For a deeper insight, the complexities unfold with mechanisms rooted in the very framework of our cellular makeup.
how diabetes transforms plague composition
Intriguingly, the interaction between hyperglycemia and the arterial lining alters the chemistry of atherosclerotic plaques significantly. In patients with diabetes, studies reveal a marked reduction in collagen, an essential component crucial for plaque stability. This decline, observed in diabetic arterial plaques, is often linked to altered metabolic and inflammatory responses, exacerbating the risk of rupture. Researchers have established that decreased levels of transforming growth factor-ß are central to these modifications, leading to a frail plaque architecture more susceptible to complications like heart attacks and strokes. The interplay between transforming growth factor-ß2 and vascular smooth muscle cells underscores this transition, highlighting a pathway eager for therapeutic intervention.
future therapeutic avenues
The exploration of therapeutic strategies targeting the stabilization of atherosclerotic plaques in type 2 diabetes is a promising frontier, rich with possibilities. Enhancing the action of transforming growth factor-ß2 may offer an avenue to fortify plaque stability by promoting robust collagen deposition and effective cellular differentiation. Addressing metabolic disorders that exacerbate these processes reveals opportunities for breakthroughs in individualized care strategies. Future research may unlock potential pathways, offering not just a mitigation of risk but also a transformation in how we combat the compounded threats of cardiovascular disease in patients battling diabetes.